Did you know that individuals with fibromyalgia often experience gut problems alongside their chronic pain and fatigue? It’s a lesser-known aspect of this debilitating condition, but one that can significantly impact a person’s quality of life. In this blog post, we will delve into the connection between fibromyalgia and gut problems, exploring the potential causes and discussing strategies for managing these symptoms. Whether you’re someone living with fibromyalgia or simply interested in learning more, this post will provide valuable insights into a frequently overlooked aspect of the condition.
The Link Between Fibromyalgia and Gut Problems
Living with fibromyalgia can be challenging enough, but when gut problems enter the picture, it can make daily life even more difficult. Many individuals with fibromyalgia report symptoms such as irritable bowel syndrome (IBS), bloating, constipation, diarrhea, and abdominal pain. While the exact relationship between fibromyalgia and gut problems is still being researched, several theories suggest a potential connection:
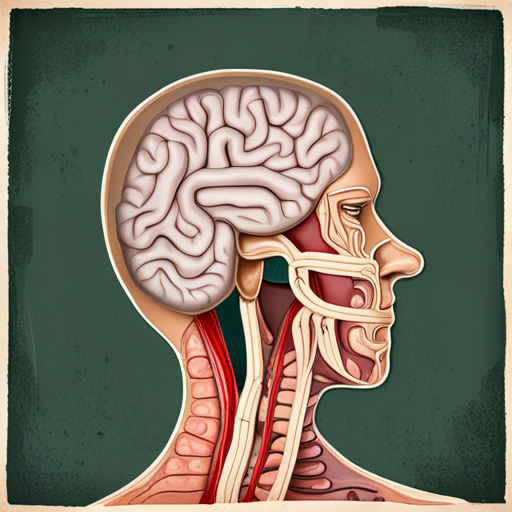
Gut-Brain Axis Dysfunction
The gut-brain axis refers to the bidirectional communication system between the gut and the brain. It involves various complex pathways, including the nervous system, immune system, hormones, and gut microbiota. Studies have indicated that individuals with fibromyalgia may experience dysfunction in this axis, leading to gut problems and other associated symptoms.
Possible Causes of Gut Problems in Fibromyalgia
While the exact cause of gut problems in fibromyalgia is not yet fully understood, several factors may contribute to the development of these symptoms:
Gut Dysbiosis
Gut dysbiosis refers to an imbalance in the gut microbiota, which are the trillions of microorganisms residing in our digestive tract. Research suggests that individuals with fibromyalgia may have an altered gut microbiome composition, with lower levels of beneficial bacteria and higher levels of harmful bacteria. This imbalance can lead to gut inflammation, increased intestinal permeability (leaky gut), and potentially trigger symptoms such as IBS.
Hypersensitivity of Nerves
In fibromyalgia, individuals often experience heightened sensitivity to pain, known as central sensitization. This hypersensitivity can extend to the nerves in the gastrointestinal tract, leading to increased pain perception and altered gut motility. The overstimulation of these nerves can contribute to symptoms such as abdominal pain, bloating, and changes in bowel habits.
Managing Gut Problems in Fibromyalgia
While there is no cure for fibromyalgia or its associated gut problems, there are strategies that can help alleviate symptoms and improve overall well-being:
Healthy Diet and Lifestyle Modifications
Adopting a healthy diet that includes plenty of fiber-rich foods, such as fruits, vegetables, and whole grains, can support gut health and regular bowel movements. Avoiding trigger foods, such as those high in fat, caffeine, and artificial additives, may also help reduce gut symptoms. Additionally, practicing stress management techniques, getting regular exercise, and ensuring adequate sleep can contribute to better gut function.
Probiotics and Prebiotics
Supplementing with probiotics (live beneficial bacteria) and prebiotics (food for these bacteria) may help restore a healthy gut microbiome balance. Probiotics can be found in fermented foods like yogurt, kimchi, and sauerkraut, or in supplement form. Prebiotics, on the other hand, are found in foods like garlic, onions, bananas, and whole grains.
Medications and Therapies
In some cases, medications may be prescribed to manage specific gut symptoms, such as antispasmodics for IBS-related pain or laxatives for constipation. Additionally, therapies such as cognitive-behavioral therapy (CBT) or gut-directed hypnotherapy may help individuals with fibromyalgia manage their gut problems by addressing the underlying psychological factors that contribute to symptom exacerbation.
The Impact of Gut Problems on Fibromyalgia
Fibromyalgia is a complex and multifaceted condition that affects not only the musculoskeletal system but also various other aspects of a person’s health. One significant area of impact is the gut. Gut problems in fibromyalgia can exacerbate the already existing symptoms and contribute to a vicious cycle of pain, fatigue, and digestive distress. Understanding the connection between fibromyalgia and gut problems is crucial for finding effective management strategies and improving overall well-being.
Exploring Potential Treatments and Therapies
Managing gut problems in fibromyalgia requires a comprehensive approach that addresses the underlying causes and provides symptom relief. While there is no one-size-fits-all solution, several treatments and therapies have shown promise in alleviating gut symptoms and improving quality of life for individuals with fibromyalgia. These include dietary modifications, probiotics and prebiotics, medications, and various therapeutic approaches tailored to address the specific needs of each individual.
Understanding the Role of Stress and Mental Health
Stress and mental health play a significant role in both fibromyalgia and gut problems. High levels of stress can exacerbate fibromyalgia symptoms and contribute to gut dysregulation, while gut problems can also generate stress and impact mental well-being. Addressing stress through relaxation techniques, therapy, and self-care practices can help manage both fibromyalgia and gut symptoms. Additionally, addressing any underlying mental health conditions can have a positive impact on overall symptom management and well-being.
Building a Supportive Lifestyle and Network
Living with fibromyalgia and gut problems can be isolating and challenging, but building a supportive lifestyle and network can make a significant difference. Connecting with others who understand the challenges of fibromyalgia and gut problems can provide emotional support, practical advice, and a sense of belonging. Engaging in activities that bring joy, practicing self-care, and seeking professional support when needed are all essential components of building a lifestyle that supports overall well-being.
Conclusion
In conclusion, gut problems are a common and often overlooked aspect of fibromyalgia. The intricate connection between fibromyalgia and the gut highlights the need for a comprehensive approach to managing symptoms and improving overall well-being. By understanding the potential causes, exploring effective treatments, addressing stress and mental health, and building a supportive lifestyle, individuals with fibromyalgia can find relief from gut problems and enhance their quality of life. Remember, each person’s experience with fibromyalgia is unique, so it’s important to work closely with healthcare professionals to develop a personalized treatment plan that meets individual needs. With persistence and support, it is possible to manage fibromyalgia and find relief from gut problems.