Did you know that there may be a link between fibromyalgia and gut dysbiosis? Fibromyalgia is a complex chronic pain condition that affects millions of people worldwide. It is characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances. On the other hand, gut dysbiosis refers to an imbalance in the gut microbiota, the trillions of microorganisms that reside in our digestive system. In recent years, researchers have been investigating the potential connection between these two conditions, and the findings are fascinating. In this blog post, we will dive into the topic of fibromyalgia and gut dysbiosis, exploring the possible relationship and its implications.
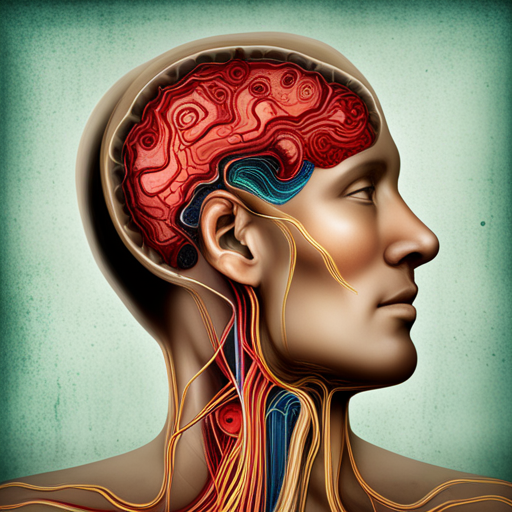
The Gut-Brain Axis: A Complex Communication Network
The gut and the brain are intricately connected through a bidirectional communication pathway called the gut-brain axis. This axis involves a complex network of nerves, hormones, and biochemical signaling molecules that facilitate communication between the gut and the brain. The gut microbiota plays a crucial role in this communication network, influencing various physiological processes and even impacting mental health and cognitive function.
The Gut Microbiota and Fibromyalgia
Emerging research suggests that alterations in the gut microbiota may contribute to the development and progression of fibromyalgia. Studies have found significant differences in the gut microbiota composition of individuals with fibromyalgia compared to healthy individuals. These differences include a decrease in beneficial bacteria, such as Bifidobacterium and Lactobacillus, and an increase in potentially harmful bacteria, such as Clostridium and Streptococcus.
The gut microbiota is responsible for various functions, including digestion, nutrient metabolism, immune system modulation, and the production of neurotransmitters. Imbalances in the gut microbiota, known as dysbiosis, can lead to increased intestinal permeability, systemic inflammation, and altered neurotransmitter levels—all of which have been implicated in fibromyalgia.
The Role of Intestinal Permeability
Intestinal permeability, also known as “leaky gut,” refers to an increased permeability of the intestinal lining, allowing substances that should be restricted to enter the bloodstream. Research suggests that individuals with fibromyalgia may have higher levels of intestinal permeability, which can lead to the entry of bacteria and their byproducts into the bloodstream. This can trigger an immune response and chronic inflammation, contributing to the pain and other symptoms experienced in fibromyalgia.
The Gut-Brain Connection: Neurotransmitters and Fibromyalgia
The gut microbiota also plays a crucial role in the production and regulation of neurotransmitters, the chemical messengers that transmit signals between nerve cells in the brain. Research has shown that imbalances in neurotransmitter levels are associated with fibromyalgia and its symptoms.
Serotonin and Fibromyalgia
Serotonin is a neurotransmitter that regulates mood, sleep, and pain perception. Studies have found that individuals with fibromyalgia often have lower levels of serotonin in their brains. Interestingly, the majority of serotonin in the body is produced in the gut, specifically by certain bacteria in the gut microbiota. Therefore, an imbalance in the gut microbiota could potentially lead to decreased serotonin production, contributing to the development and severity of fibromyalgia symptoms.
Impact of Serotonin on Pain Perception
Serotonin is known to play a role in modulating pain perception. Reduced serotonin levels can lead to an increased sensitivity to pain, a common symptom in fibromyalgia. Additionally, serotonin is involved in regulating sleep, and disrupted sleep patterns are a hallmark of fibromyalgia. Restoring a healthy balance in the gut microbiota and promoting serotonin production may help alleviate pain and improve sleep in individuals with fibromyalgia.
The Gut Microbiota and Treatment Approaches
Given the potential connection between fibromyalgia and gut dysbiosis, researchers are exploring treatment approaches that target the gut microbiota to alleviate fibromyalgia symptoms.
Probiotics and Prebiotics
Probiotics are live bacteria that confer health benefits when consumed in adequate amounts. Several studies have investigated the use of probiotics in individuals with fibromyalgia, and while the results are promising, more research is needed to establish their effectiveness.
Prebiotics, on the other hand, are non-digestible fibers that promote the growth and activity of beneficial bacteria in the gut. Incorporating prebiotic-rich foods, such as fruits, vegetables, and whole grains, into the diet may help restore a healthy gut microbiota and alleviate fibromyalgia symptoms.
Diet and Lifestyle Modifications
In addition to probiotics and prebiotics, adopting a healthy diet and lifestyle can support a balanced gut microbiota. This includes consuming a variety of plant-based foods, avoiding processed foods and excessive sugar intake, managing stress levels, and getting regular exercise.
The Impact of Stress on Gut Dysbiosis and Fibromyalgia
Stress is known to have a significant impact on both gut health and fibromyalgia. Chronic stress can disrupt the balance of the gut microbiota, leading to dysbiosis. On the other hand, individuals with fibromyalgia often experience heightened stress levels, which can further exacerbate their symptoms. The interplay between stress, gut dysbiosis, and fibromyalgia is a complex relationship that requires further investigation.
The Role of Stress on Gut Dysbiosis
Stress triggers the release of stress hormones such as cortisol, which can negatively affect the gut microbiota. Studies have shown that chronic stress can lead to imbalances in the gut microbiota composition, favoring the growth of harmful bacteria and reducing beneficial bacteria. This dysbiosis can contribute to a variety of gastrointestinal symptoms and may also have systemic effects on overall health.
Stress as a Trigger for Fibromyalgia Flares
Fibromyalgia is a condition characterized by heightened sensitivity to pain, and stress has been identified as a common trigger for fibromyalgia flares. The physiological response to stress can lead to increased inflammation and pain perception, worsening fibromyalgia symptoms. Managing stress through techniques such as relaxation exercises, mindfulness, and therapy may help reduce the severity of fibromyalgia symptoms and restore gut health.
Conclusion
In conclusion, there appears to be a link between fibromyalgia and gut dysbiosis. The gut microbiota plays a crucial role in maintaining overall health, and imbalances in the gut microbiota have been implicated in the development and progression of fibromyalgia. Altered intestinal permeability, neurotransmitter imbalances, and the impact of stress are all potential mechanisms through which gut dysbiosis may contribute to fibromyalgia symptoms.
While more research is needed to fully understand the relationship between fibromyalgia and gut dysbiosis, there are steps individuals can take to support gut health and potentially alleviate fibromyalgia symptoms. Incorporating probiotics and prebiotics into the diet, adopting a healthy lifestyle, managing stress levels, and seeking professional guidance are all important strategies to consider.
By addressing gut dysbiosis and promoting a healthy gut microbiota, individuals with fibromyalgia may find relief from their symptoms and improve their overall well-being. It is an exciting area of research that holds promise for the future of fibromyalgia treatment.