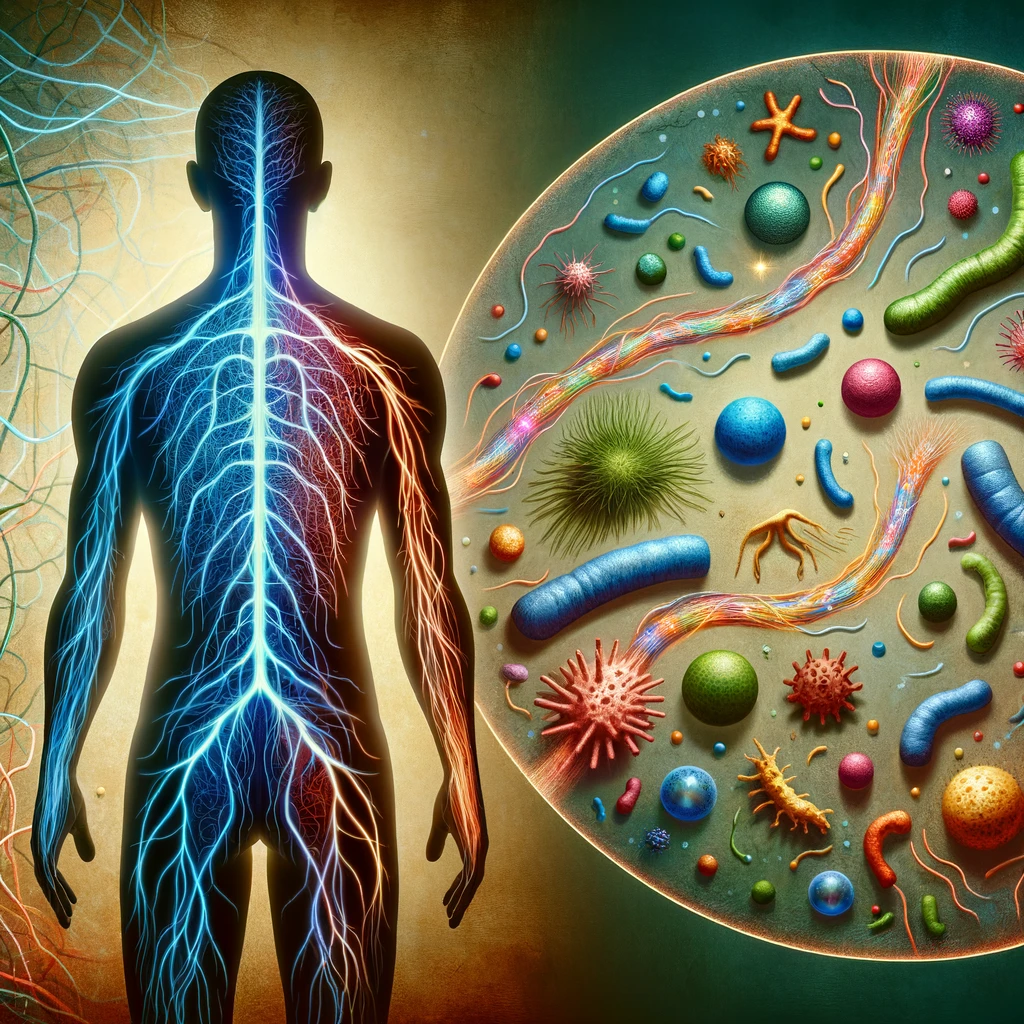
Are you one of the millions of people living with fibromyalgia, a chronic pain condition that affects the muscles and joints? If so, you may be interested to learn about the emerging research on the potential connection between fibromyalgia and the gut microbiome. While fibromyalgia has long been believed to be a disorder of the nervous system, recent studies suggest that the gut microbiome, the collection of bacteria and other microorganisms in the digestive tract, may play a significant role in the development and management of fibromyalgia symptoms.
The gut microbiome is a complex ecosystem that consists of trillions of microorganisms, including bacteria, viruses, and fungi. It is known to play a crucial role in various aspects of human health, including digestion, metabolism, and immune function. Recent research has also revealed that the gut microbiome has a bidirectional relationship with the brain, influencing both physical and mental health.
Several studies have found alterations in the gut microbiome composition of individuals with fibromyalgia compared to those without the condition. These findings have sparked interest and raised important questions about the potential role of the gut microbiome in fibromyalgia pathogenesis and symptom severity. Understanding this connection could pave the way for new therapeutic approaches and improve the quality of life for individuals living with fibromyalgia.
In this blog post, we will delve into the current research on the link between fibromyalgia and the gut microbiome. We will explore the potential mechanisms underlying this connection and discuss the implications for fibromyalgia management. Furthermore, we will examine the potential therapeutic strategies targeting the gut microbiome that may offer relief for individuals with fibromyalgia. So, let's dive into the fascinating world of fibromyalgia and the gut microbiome!
The Gut Microbiome: A Key Player in Human Health
The Composition and Diversity of the Gut Microbiome
The gut microbiome is a bustling community of microorganisms that reside in the gastrointestinal tract, primarily the large intestine. It is estimated to consist of trillions of microorganisms, including bacteria, viruses, fungi, and other microscopic organisms. Collectively, these microorganisms make up a diverse and complex ecosystem that interacts with our bodies in numerous ways.
The composition of the gut microbiome can vary significantly among individuals, influenced by factors such as genetics, diet, age, geographic location, and medication use. While there is no "one-size-fits-all" gut microbiome, certain bacterial species are more prevalent in healthy individuals, contributing to a balanced and resilient microbial community.
Gut Microbiome and its Role in Human Health
The gut microbiome plays a crucial role in maintaining our overall health and well-being. It is involved in several essential functions, including:
1. Digestion and Nutrient Absorption:
The gut microbiome helps break down complex carbohydrates, fibers, and other indigestible compounds that our own digestive enzymes cannot process. As a result, these microorganisms produce essential nutrients, such as short-chain fatty acids, that nourish the cells lining the gut and provide energy for our body.
2. Immune Function:
The gut microbiome plays a significant role in training and modulating our immune system. It helps educate our immune cells to differentiate between harmful pathogens and harmless substances, preventing unnecessary immune responses and reducing the risk of autoimmune diseases.
3. Metabolism and Weight Regulation:
Studies have shown that the gut microbiome can influence our metabolism and regulate body weight. Certain bacterial species in the gut microbiome are associated with increased energy extraction from food, leading to weight gain, while others promote a lean phenotype and help prevent obesity.
4. Mental Health and Brain Function:
Emerging research suggests a strong bidirectional communication between the gut microbiome and the brain, known as the gut-brain axis. The gut microbiome produces neurotransmitters and other signaling molecules that can influence brain function, mood, and behavior. Imbalances in the gut microbiome composition have been linked to mental health disorders, including depression, anxiety, and stress-related conditions.
These are just a few examples of the extensive influence the gut microbiome has on our health. Now, let's explore the intriguing link between the gut microbiome and fibromyalgia and how it may impact the development and management of this chronic pain condition.
The Gut Microbiome and Fibromyalgia: Exploring the Connection
Altered Gut Microbiome Composition in Fibromyalgia
Several studies have observed significant differences in the gut microbiome composition between individuals with fibromyalgia and those without the condition. These alterations involve changes in the abundance and diversity of certain bacterial species.
One study published in the journal Pain found that individuals with fibromyalgia had lower levels of beneficial bacteria, such as Faecalibacterium and Bifidobacterium, compared to healthy controls. These bacteria are known to have anti-inflammatory properties and play a role in maintaining a healthy gut environment.
Another study published in the journal Scientific Reports discovered a reduction in microbial diversity in fibromyalgia patients. Microbial diversity refers to the variety of different bacterial species present in the gut. A decrease in microbial diversity has been associated with various health conditions and is considered a marker of gut dysbiosis, an imbalance in the gut microbiome.
These findings suggest that fibromyalgia may involve disruptions in the delicate balance of the gut microbiome, potentially contributing to the development and progression of the condition. However, more research is needed to understand the specific mechanisms underlying these alterations and their impact on fibromyalgia symptoms.
The Gut Microbiome-Brain Axis and Fibromyalgia
One of the key mechanisms through which the gut microbiome may influence fibromyalgia is via the gut-brain axis. The gut-brain axis is a bidirectional communication pathway that involves the constant exchange of signals between the gut and the central nervous system.
The gut microbiome produces a wide range of molecules and metabolites that can directly or indirectly affect brain function and behavior. These molecules include neurotransmitters, such as serotonin and dopamine, as well as short-chain fatty acids and bacterial toxins.
Emerging evidence suggests that imbalances in the gut microbiome composition, known as dysbiosis, can lead to increased gut permeability, also known as "leaky gut." This increased permeability allows toxins and other harmful substances to enter the bloodstream, triggering an immune response and causing systemic inflammation.
Systemic inflammation has been implicated in the pathogenesis of fibromyalgia, contributing to the characteristic widespread pain and other symptoms associated with the condition. By influencing gut permeability and inflammation, the gut microbiome may play a role in the development and maintenance of fibromyalgia symptoms.
Therapeutic Approaches Targeting the Gut Microbiome in Fibromyalgia
Dietary Modifications
Diet plays a crucial role in shaping the gut microbiome, and making certain dietary modifications may help improve symptoms in individuals with fibromyalgia. Here are some dietary strategies that have shown promise:
1. Probiotics and Prebiotics:
Probiotics are live bacteria that can provide health benefits when consumed, while prebiotics are dietary fibers that serve as food for beneficial bacteria in the gut. Both probiotics and prebiotics can help restore the balance of the gut microbiome and improve gut health. Including probiotic-rich foods, such as yogurt, kefir, and sauerkraut, and prebiotic-rich foods, such as onions, garlic, and bananas, in your diet may be beneficial.
2. Fiber-Rich Foods:
Consuming an adequate amount of dietary fiber can support the growth of healthy bacteria in the gut. Whole grains, fruits, vegetables, and legumes are excellent sources of fiber that can promote a diverse and balanced gut microbiome.
3. Anti-Inflammatory Diet:
An anti-inflammatory diet, which focuses on whole, unprocessed foods and limits inflammatory foods such as refined sugars and saturated fats, may help reduce inflammation in the gut and throughout the body. This can potentially alleviate fibromyalgia symptoms.
Probiotic and Prebiotic Supplements
In addition to dietary modifications, taking probiotic and prebiotic supplements may be beneficial for individuals with fibromyalgia. These supplements can help introduce beneficial bacteria into the gut and promote the growth of healthy microbial communities. However, it's important to note that the efficacy of these supplements may vary among individuals, and it's best to consult with a healthcare professional before starting any new supplement regimen.
Antibiotics and Microbiome Transplantation
In some cases, healthcare professionals may prescribe antibiotics to individuals with fibromyalgia to target specific bacterial imbalances in the gut microbiome. While antibiotics can have a significant impact on the gut microbiome, their use should be carefully considered and guided by a healthcare professional to minimize potential risks and side effects.
Another emerging therapeutic approach is fecal microbiota transplantation (FMT). FMT involves transferring fecal matter from a healthy donor to the intestine of an individual with an imbalanced gut microbiome. This procedure aims to restore a healthy gut microbiome and has shown promising results in treating certain gastrointestinal conditions. However, more research is needed to determine the efficacy and safety of FMT for fibromyalgia.
Conclusion
The emerging research on the connection between the gut microbiome and fibromyalgia opens up new possibilities for understanding and managing this chronic pain condition. Altered gut microbiome composition and dysbiosis have been observed in individuals with fibromyalgia, suggesting a potential role of the gut microbiome in its pathogenesis and symptom severity.
By targeting the gut microbiome through dietary modifications, probiotic and prebiotic supplements, antibiotics, and potentially FMT, it may be possible to alleviate fibromyalgia symptoms and improve the quality of life for individuals living with this condition.
However, it's essential to note that the research on the gut microbiome and fibromyalgia is still in its early stages, and more studies are needed to fully understand the mechanisms and establish effective therapeutic strategies. It's recommended to work with healthcare professionals who specialize in gut health and fibromyalgia to develop an individualized treatment plan.
As research continues to unravel the fascinating link between the gut microbiome and fibromyalgia, there is hope for new and innovative approaches to manage this complex condition. By harnessing the power of the gut microbiome, we may be able to improve the lives of millions of individuals living with fibromyalgia and pave the way for personalized and targeted therapies.